The Cornerstone of Quality Patient Care
In the fast-paced world of healthcare, clear and concise documentation is the cornerstone of providing quality patient care. This documentation contains SOAP notes (subjective, objective, assessment, plan). They are structured in a specific format. They let physicians and others capture patient encounters, clinical findings, and treatment plans. Healthcare professionals must master the art of writing effective SOAP notes to enhance clinical efficiency, ensure legal compliance, and improve patient outcomes.
Understanding the direct impact of effective SOAP note documentation on clinical outcomes reveals its significance. For instance, doctors with strong documentation skills use the SOAP charting method. They see an increase in clinical efficiency scores. This increase is associated with higher quality patient care.
This guide will explore the definition of SOAP notes, details on writing them effectively, best practices, technology integration, and strategies for overcoming common challenges. By the end, readers will have the knowledge and tools to improve their SOAP note documentation. It will raise quality, speed up patient care, and protect against legal risks.
Best Practices in SOAP Note Documentation
When it comes to documenting patient care, following the best practices and using SOAP notes examples as references can make a big difference. This helps healthcare professionals streamline their documentation process and improve communication across the entire care team.
Legal Considerations: Ensuring Compliance
Meticulous SOAP note documentation is crucial for legal protection and compliance with healthcare regulations. To mitigate legal risks:
- Ensure SOAP notes reflect the patient encounter and clinical decision-making process.
- Document any deviations from standard treatment protocols, including the rationale for such deviations.
- Maintain detailed records of informed consent processes and discussions with patients or caregivers.
Adhering to legal best practices not only protects healthcare professionals but also safeguards patient rights and upholds the integrity of the healthcare system.
Confidentiality and Security: Protecting Patient Information
Preserving patient confidentiality is a fundamental ethical principle in healthcare. Robust security measures, such as encryption and access controls, can reduce data breaches. To safeguard patient privacy:
- Use secure electronic medical record (EMR) systems for storing and sharing SOAP notes.
- Implement strict access controls, limiting access to SOAP notes on a need-to-know basis.
- Avoid including sensitive patient information in SOAP notes unless necessary for clinical decision-making.
By prioritizing confidentiality and security, healthcare professionals foster trust and maintain the integrity of the patient-provider relationship.
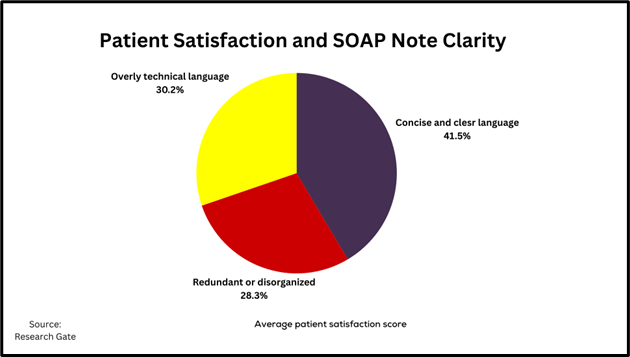
Clarity and Conciseness: Enhancing Readability
Clear and concise writing is essential for effective communication in SOAP notes. Physicians who avoid redundancy and technical language have a higher patient satisfaction rating. To improve readability:
- Use simple, straightforward language whenever possible.
- Employ bullet points or numbered lists to organize information logically.
- Utilize headings and subheadings to break up lengthy sections.
- Proofread carefully to eliminate spelling and grammatical errors.
By prioritizing clarity and conciseness, SOAP notes become more accessible and valuable resources for both healthcare professionals and patients.
Structuring Your SOAP Note: The Building Blocks
Now that the critical role of adept SOAP note documentation has been established, let’s delve into crafting each component of the SOAP note format for maximum effectiveness.
Subjective: Capturing the Patient’s Story
The Subjective section sets the stage for the entire SOAP note by capturing the patient’s narrative or soap narrative example. Healthcare professionals use open-ended questions to get full patient histories.
To craft an effective Subjective section:
- Use active listening techniques to encourage patients to share their concerns and symptoms.
- Document the patient’s statements verbatim, avoiding bias or interpretation.
- Probe for additional details, such as the onset, duration, and severity of symptoms.
By capturing the patient’s story, you lay the groundwork for a thorough assessment and tailored treatment plan.
Objective: Clinical Findings and Observations
The Objective section documents measurable clinical data, including vital signs, physical examination findings, and test results.
To ensure accurate and comprehensive Objective documentation:
- Record all relevant vital signs, including temperature, blood pressure, pulse, and respiratory rate.
- Describe physical examination findings in detail, using precise medical terminology.
- Document the results of any diagnostic tests or procedures performed.
Objectivity and precision in this section are paramount, as these clinical findings inform the subsequent assessment and treatment plan.
Assessment: Making Clinical Judgments
In the Assessment section, healthcare professionals synthesize the Subjective and Objective information to formulate a clinical impression or diagnosis.
To craft an insightful Assessment:
- Analyze the patient’s symptoms and clinical findings to identify potential underlying conditions.
- Consider and document relevant differential diagnoses, explaining the rationale for ruling them in or out.
- Clearly state the primary diagnosis or clinical impression.
A well-articulated Assessment section not only aids in accurate diagnosis but also facilitates continuity of care among healthcare teams.
Plan: Mapping Out the Treatment Strategy
The Plan section outlines the course of action for addressing the patient’s condition, including medications, therapies, follow-up appointments, and any necessary referrals.
To create an effective Plan section of the soap note:
- Specify any medications prescribed, including dosages, routes, and durations.
- Detail any therapies, procedures, or diagnostic tests ordered.
- Communicate follow-up instructions, including the date and reason for the next appointment.
- Tailor the plan to the patient’s specific needs and preferences.
A well-crafted Plan section empowers patients to participate in their care, fostering better health outcomes.
Leveraging Technology in SOAP Note Writing
In the evolving healthcare environment, technology offers powerful tools to streamline and enhance SOAP note documentation. Integration of Electronic Health Records (EHR) with SOAP note processes can reduce documentation time.
EHR and SOAP Note Software
Numerous EHR systems and dedicated SOAP note software solutions are available to healthcare professionals. Popular options include:
- DrChrono: A cloud-based EHR platform with SOAP note templates and voice-to-text capabilities.
- Athenahealth: An integrated EHR suite featuring customizable SOAP note templates and mobile accessibility.
- Epic: A comprehensive EHR system used by large healthcare organizations, with robust SOAP note functionality.
Physicians currently use EHR-integrated tools for SOAP note documentation, recognizing the efficiency and accuracy benefits they provide.
Benefits of EHR Integration
Integrating SOAP note processes with EHR systems offers several advantages:
- Streamlined Workflow: EHRs allow for seamless documentation during patient encounters, reducing the need for separate note-taking.
- Automated Data Retrieval: Patient history, test results, and other relevant data can be populated, reducing manual entry.
- Standardization: EHRs enforce consistent formatting and terminology, improving clarity and reducing errors.
- Accessibility: SOAP notes can be accessed and shared among healthcare teams, facilitating continuity of care.
By embracing technology, healthcare professionals can optimize their SOAP note documentation processes, freeing up valuable time to focus on delivering high-quality patient care.
Common Challenges and Solutions
Despite the benefits of structured SOAP note documentation and technological advancements, healthcare professionals often encounter specific recurring challenges. Addressing these challenges can further enhance the quality and efficiency of SOAP note writing.
Time Constraints and Incomplete Information
One of the most common challenges in SOAP note documentation is the pressure of time constraints and incomplete patient information. To overcome these obstacles, consider implementing the following solutions:
- Voice-to-Text Dictation: Utilizing speech recognition software can reduce the time required for manual data entry.
- Automated Data Retrieval: As mentioned earlier, EHR systems can populate patient histories, test results, and other relevant data, minimizing the need for manual information gathering.
- Templating: Customizable SOAP note templates can provide a structured framework, reducing the time spent organizing documentation.
- Prioritizing Information: When faced with incomplete data, focus on documenting the most pertinent details first, and make a plan to follow up on missing information.
Healthcare professionals can streamline their documentation process by using these solutions, even when faced with time pressures or incomplete patient records.
Common Documentation Errors
Errors in SOAP note documentation can have far-reaching consequences, including compromised patient care and legal liabilities. According to the Journal of Healthcare Management, some of the most common mistakes include:
- Incomplete or missing information
- Lack of specificity in descriptions
- Poor organization and flow of information
- Inconsistent terminology or abbreviations
To reduce these errors and improve SOAP note quality, healthcare organizations should implement the following strategies:
- Regular Audits: Conducting periodic audits of SOAP notes can help identify errors and areas for improvement.
- Peer Review: Encouraging a culture of peer review, where colleagues provide feedback on each other’s documentation, can help identify and correct mistakes.
- Ongoing Education: Providing regular training and educational resources on SOAP note best practices can reinforce proper techniques and keep healthcare professionals up-to-date with the latest guidelines.
By fixing common errors and adding solutions, healthcare pros can improve their SOAP note. They can improve its accuracy, consistency, and quality.
Frequently Asked Questions
1. What are the most common errors made in SOAP notes, and how can they be avoided?
Common errors in SOAP notes include missing or incomplete information. They also lack specificity, are poorly organized, and use inconsistent terms. You can reduce these errors with regular audits, peer review, and ongoing education. The Journal of Healthcare Management highlighted this.
2. How can I make my SOAP notes more useful for other healthcare professionals?
To make your SOAP notes more valuable for interprofessional communication, use standardized terms. Also, give clear and short assessments and plans. Include relevant patient history and context. The Journal of Interprofessional Care noted this. It makes collaboration and care continuity seamless.
3. Are there legal implications if SOAP notes are poorly written?
Yes, poorly written SOAP notes can have significant legal implications. Medical Economics reports that 85% of medical malpractice claims involve improper documentation. Bad SOAP notes can expose healthcare pros to liability. They can also hurt their legal defense in a lawsuit.
Conclusion
Writing effective SOAP notes is a vital skill. It’s essential for healthcare professionals dedicated to exceptional patient care. Using a structured format, best practices, and technology. By addressing common challenges, you can create clear, concise, and legally compliant documentation.
Remember, your SOAP notes are more than just records. They are narratives. They shape patient experiences, inform decisions, and protect patients and healthcare professionals. Embrace the power of effective documentation and upgrade your practice to new heights.